Rafael Sacchetti1, Bruno Coelho Mendes2, Bruno Costa Martins de Sá2, Claudio Ferreira Nóia2, Sergio Charifker Ribeiro Martins3, Leandro Lécio de Lima Sousa3 and Tarcio Hiroshi Ishimine Skiba2
Abstract
The oral rehabilitation with implant supported prosthesis it is challenging in areas where there is not enough thickness. This is the case of atrophies in the maxilla or mandible in edentulous patients. To achieve a satisfactory bone volume that allows the installation of implants, several techniques can be performed. This report presents the case of a 55-yearold female patient with insufficient bone thickness between the maxillary canines, but with a satisfactory height for implant placement. The Split crest technique was per-formed, taking advantage of the bone height and the medullary portion in the region, al-lowing the immediate installation of implants with bone graft. The postoperative period was uneventful and at 6 months it was possible to install the provisional crowns. There-fore, it is concluded that the Split crest technique is predictable and allows safe oral rehabilitation.
Keywords: Oral rehabilitation; Split crest technique; Prosthesis; Tooth Loss.
Introduction
The tooth loss is related to aesthetic, functional and social consequences. Furthermore, it results in the absence of stimuli to the alveolar bone. Stimulation of the alveolar bone is responsible for maintaining bone volume. Without stimulation the bone will undergo a process of atrophy, which is characterized in the maxilla first by the reduction in thick-ness and then by vertical resorption. In the anterior region of the maxilla, the need to re-store the anatomy to ideal conditions becomes critical, due to the great aesthetic importance of the region [1]. There are many established techniques for bone
reconstruction and anatomical restoration
of the anterior maxillary region. The split crest technique is a method of bone graft used to increase thickness, commonly indicated for this area due to the characteristic of low local density and pattern of bone resorption. To perform this technique, it is necessary that there is remaining bone in thickness, with medullary bone between the cortical bones.
[2].
In this technique, vertical osteotomies are performed to allow the splitting the alveolar ridge longitudinally in two parts. The buccal cortical bone plate is separated from the bone marrow and displaced in a labial direction to increase the alveolar ridge
width to enable insertion of implants. This technique allows the immediate installation of dental implants in the created gap,
reducing the total time of recovery for rehabilitation [3,4]. This report shows a case of split crest technique with immediate
implant placement.
Case report
A 55-year-old female patient came to the dental office complaining about the esthetics of her smile, dental absences, and
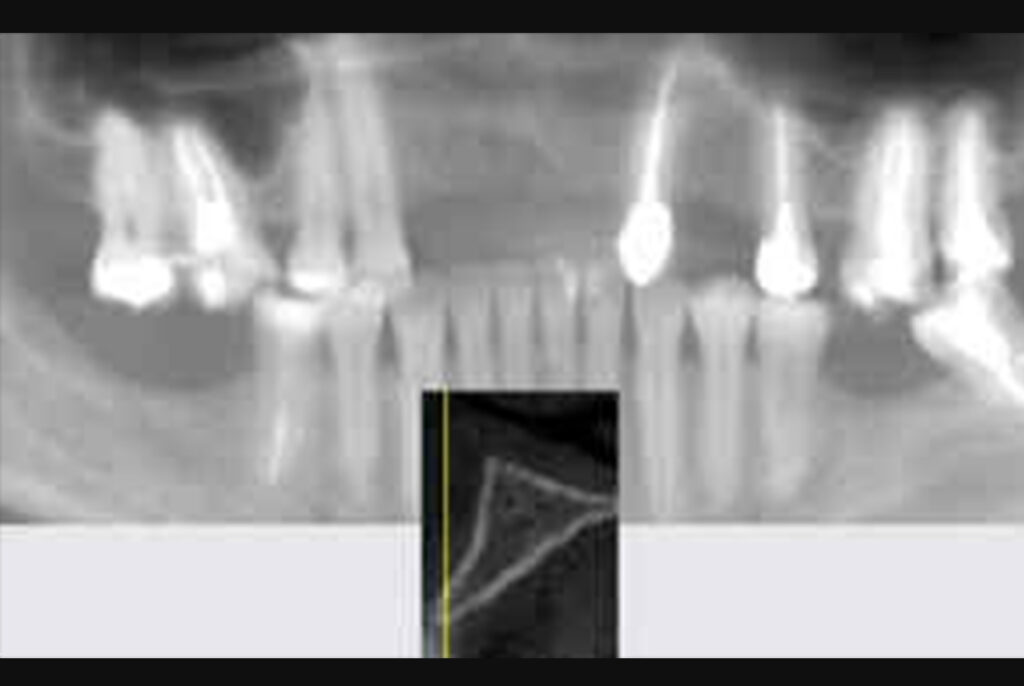
referring interest in oral rehabilitation with im-plant-supported prosthesis. The clinical exam showed absence of 4 upper incisors and horizontal bone deficiency (Figure 1, 2).
Computed tomography showed the presence of 3mm of remaining bone thickness, with medullary bone, and preservation of alveolar bone height (Figure 3). In view of the observed condition, the proposed planning was to carry out the Split Crest technique, installing 4 implants, replacing the 4 missing teeth.

Figure 1: The clinical exam showed absence of 4 upper incisors and horizontal bone deficiency.

Figure 2: The clinical exam showed absence of 4 upper incisors and horizontal bone deficiency.
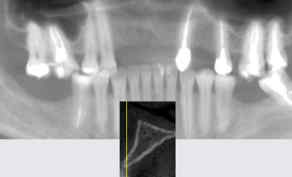
Figure 3: Computed tomography showed the presence of 3mm of remaining bone thickness, with
medullary bone, and preservation of alveolar bone height.
To perform the surgery, the rigorous process to maintain the aseptic chain was followed. Anesthesia of the anterior superior alveolar nerves and incisive nerve was per-formed bilaterally. A horizontal incision, slightly displaced towards the palatal aspect was performed on the alveolar ridge, with two vertical relaxing incisions distal to the canines. After the mucoperiosteal detachment (Figure 4), the incisive canal was emptied with a supercutting bur (Implacil De Bortoli, São Paulo, SP, Brazil) (Figure 5).
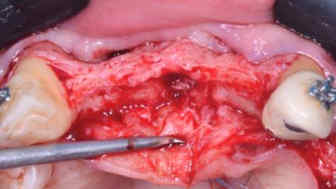
Figure 4: The mucoperiosteal detachment.

Figure 5: The incisive canal was emptied with a super-cutting bur.
Three vertical osteotomies were performed in the buccal cortical bone up to the medullary portion, at the mesial of the
canines and midline (Figure 6), followed by alveolar ridge crest osteotomy between the canines (Figure 7). All osteotomies were performed under abundant irrigation with saline solution. Subsequently, the surgical guide was tested, observing the positioning of each implant (Figure 8).

Figure 6: Three vertical osteotomies were performed in the buccal cortical bone up to the medullary
portion, at the mesial of the canines and midline.

Figure 7: Alveolar ridge crest osteotomy between the canines.

Figure 8: Testing of Surgical Guide.
The crest division was performed with the aid of chisels (Figure 9) and with digital rotary expanders (Supremo surgical
instruments, Sp, Brazil) installed with a ratchet, evolving from the smallest to the largest caliber until obtaining 3.3 mm in
diameter (Figure 10 and 11). The bone expansion obtained was sufficient for the installation of Osseo integrated implants at
the same surgery at the sites of teeth 11, 12, 21, and 22 (Figure 12, 13). After that, the gaps were filled with particulate bone graft Lumina Bone Porous large (Criteria Biomateriais, São Carlos, SP, Brazil) (Figure 14, 15, 16) being covered with calcium sulfate hemihydrate Lumina Set (Criteria Biomateriais, São Carlos, SP, Brazil) (Figure 17), in order to optimize the stability of the bone graft. Subsequently, the surgical site was covered with a resorbable membrane Lumina Coat double time (Criteria Biomateriais, São Carlos, SP, Brazil) (Figure 18, 19, 20). The suture was performed after periosteum incision for flap release. It was performed with polypropylene thread (Microsuture, São Paulo, SP, Brazil) (Figure 21, 22), with two horizontal mattress sutures for approximation of edges and simple stitches until complete closure of the flap.
The post-operative period was uneventful. The 6 months postoperative computed tomography (Figure 23) shows the optimal placement of implants (Figure 24), allowing the reopening and installation of provisional crowns.

Figure 9: The crest division was performed with the aid of chisels.

Figure 10: Digital rotary expanders installed.
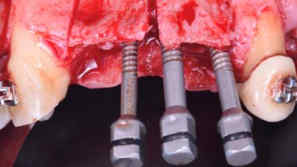
Figure 11: Digital rotary expanders installed.

Figure 12: The bone expansion obtained for the installation of Osseo integrated implants.

Figure 13: The bone expansion obtained for the installation of Osseo integrated implants.

Figure 14: The gaps were filled with particulate bone graft Lumina Bone Porous large.

Figure 15: The gaps were filled with particulate bone graft Lumina Bone Porous large.

Figure 16: The gaps were filled with particulate bone graft Lumina Bone Porous large.

Figure 17: The gaps were filled with particulate bone graft Lumina Bone Porous large covered with
calcium sulfate hemihydrate Lumina Set.

Figure 18: The surgical site was covered with a resorbable membrane Lumina Coat double time.

Figure 19: The surgical site was covered with a resorbable membrane Lumina Coat double time.

Figure 20: The surgical site was covered with a resorbable membrane Lumina Coat double time.

Figure 21: The suture was performed after periosteum with polypropylene thread.

Figure 22: The suture was performed after periosteum with polypropylene thread.

Figure 23: The 6 months postoperative computed tomography shows the optimal placement of
implants.

Figure 24: The 6 months image shows the optimal placement of implants.
Discussion
The technique initially described by Simion et al, in 1992, consists of performing vertical osteotomies joined by a horizontal osteotomy over the alveolar ridge. The initial technique used chisels to promote a greenstick fracture, keeping the apical portion together. Using rotary expanders, the cortical bone is moved away until it is possible to position the implant in the provided gap. A limitation of this technique is the absence of medullary bone, in order to be possible, the technique needs to be performed preferably in bone type 3 and 4 with a minimum of 3 millimeters of remaining bone tissue [5,6].
This is because the bone is more flexible and vascularized, reducing the risk of fracture due to its flexibility and ease of
revascularization. Immediate implant placement and bone expansion is well accepted in the literature, with a success rate ranging from 91.7% to 100%, which is compatible with the success rate of other grafting techniques [7,8]. The gain in bone
width in the graft region is on average 2.97 mm, thus achieving good bone thick-ness and, consequently, a good aesthetic
appearance [9]. The gap formed between the bone boards after expansion presents less bone resorption if filled with bone graft and covered with resorbable membrane, when compared to the split crest technique without graft [10]. The use of calcium sulfate as a barrier helps to limit the invasion of connective tissue in the graft, allowing bone regeneration at the surgical site [11].
Conclusion
The split crest technique is a viable alternative for cases of horizontal bone resorption, mainly because it presents the
possibility of bone grafting with the immediate installation of Osseo integrated implants.
Skiba THI | Volume 4; Issue 2 (2022) | Mapsci-JDOS-4(2)-127 | Case Report
Citation: Sacchetti R, Mendes BC, Martins de Sá BC, Nóia CF, Martins SCR, Sousa LLL, et al. Split Crest Technique for Horizontal Alveolar Augmentation and Simultaneous Dental Implant Placement: A Case Report. J Dent Oral Sci. 2022;4(2):1-10. DOI: https://doi.org/10.37191/Mapsci-2582-3736-4(2)-127
References
1. Skiba TH, Barbosa SA, Moreira Mz, De Sá BC, Nóia CF. Dental implants: case report. J Braz Coll Oral
Maxillofac Surg. 2018;4(2):59-63.
2. Waechter J, Leite FR, Nascimento GG, Carmo Filho LC, Faot F. The split crest technique and dental
implants: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2017;46(1):116-28. PubMed |
CrossRef
3. Simion M, Baldoni M, Zaffe D. Jawbone enlargement using immediate implant placement associated with a
split-crest technique and guided tissue regeneration. Int J Periodontics Restorative Dent. 1992;12(6).
PubMed
4. Bomfim B, Oliveira Júnior HC, Sá BC, Ortega-Lopes R, Nóia CF. Surgical expansion of the alveolar ridge case
report. Full Teeth Sci. 2017:10-4.
5. Vercellotti T. Piezoelectric surgery in implantology: a case report–a new piezoelectric ridge expansion
technique. Int J Periodontics Restorative Dent. 2000;20(4). PubMed
6. Suh JJ, Shelemay A, Choi SH, Chai JK. Alveolar ridge splitting: a new microsaw technique. Int J Periodontics
Restorative Dent. 2005;25(2). PubMed
7. Bassetti MA, Bassetti RG, Bosshardt DD. The alveolar ridge splitting/expansion technique: a systematic
review. Clin Oral Implants Res. 2016;27(3):310-24. PubMed | CrossRef
8. Buser D, Janner SF, Wittneben JG, Brägger U, Ramseier CA, Salvi GE. 10‐year survival and success rates of
511 titanium implants with a sandblasted and acid‐etched surface: a retrospective study in 303 partially
edentulous patients. Clin Implant Dent Relat Res. 2012;14(6):839-51. PubMed | CrossRef
9. de Souza CS, de Sá BC, Goulart D, Guillen GA, Macêdo FG, Nóia CF. Split crest technique with immediate
implant to treat horizontal defects of the alveolar ridge: analysis of increased thickness and implant survival.
J Maxillofac Oral Surg. 2020;19(4):498-505. PubMed | CrossRef
10. Ella B, Laurentjoye M, Sedarat C, Coutant JC, Masson E, Rouas A. Mandibular ridge expansion using a
horizontal bone-splitting technique and synthetic bone substitute: an alternative to bone block grafting?.
Int J Oral Maxillofac Implants. 2014;29(1). PubMed | CrossRef
11. Pecora G, Andreana S, Margarone III JE, Covani U, Sottosanti JS. Bone regeneration with a calcium sulfate
barrier. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84(4):424-9. PubMed | CrossRef.
1Department of Implantology, Cora Vilhena.
2Department of Implantology – SOEP (Sistema Odontológico de Estudos e Pesquisa).
3Department of Implantology and Periodontology RIDGE (Research Implant Dentistry and Graft Expertise) / ICS FUNORTE.
*Corresponding Author: Tarcio Hiroshi Ishimine Skiba, SOEP – Rua Elias Gorayeb 920, Nossa Sra. Das Graças, Porto Velho, RO – Brasil.
Receiving Date: 05-05-2022
Revised Date: 05-10-2022
Accepted Date: 05-16-2022
Published Date: 05-23-2022
Copyright© 2022 by Sacchetti R, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.