João Carlos Vicente de Barros Junior2, Daniela Martens Fernandes2, Ana Andrea Fonseca Rosendo de
Melo1, Danielle Oliveira Vieira1, Makeler Rampos Polassi1, Itala Caroline da Rocha Albuquerque1,
Leandro Lécio de Sousa1, Sergio Charifker Ribeiro Martins1, Bruno Costa Martins de Sá1 and
Tarcio Hiroshi Ishimine Skiba2*
1Department of Implantology and Periodontology RIDGE (Research Implant Dentistry and Graft Expertise) / ICS FUNORTE, Brazil.
2Department of Implantology and Periodontology SOEP – Dental Study and Research System / ICS FACSET, Brazil.
*Corresponding Author: Tarcio Hiroshi Ishimine Skiba, Rua Ernesto de Paula Santos, 187 – Segundo Andar, Boa Viagem – Recife, PE (Brazil) CEP:51021-330
DOI: https://doi.org/10.58624/SVOADE.2023.04.0124
Received: February 22, 2023 Published: March 10, 2023
Abstract
Aim: The goal of this paper is to describe a clinical case in which a split bone block (SBB) technique was used for a vertical augmentation of an anterior maxillary area prior to an implant based prosthetic rehabilitation. The augmentation
technique is reported in this article in addition to a discussion.
Materials and methods: A 30-year-old female was referred for an implant restauration in the left upper canine area.
After a clinical and radiographical evaluation it was decided that there was a vertical bone deficiency so that a vertical
augmentation procedure should be performed before the implant installation. A Split Bone Block technique was the
surgery of choice for that purpose.
Conclusion: The SBB technique has proven to be a predictable and reliable procedure in cases of vertical augmentation.
Keywords: vertical augmentation, implant, autografts, reconstructive surgery
Introduction
In the daily practice, it is not unusual for the practitioner to deal with cases in which there is not enough bone volume to
install dental implants and consequently set an implant based prothesis [1-4.] In order to reach that goal, a bone augmentation procedure prior to the dental implant installation becomes mandatory [1,3].
The osseous volume deficiency occurs as consequence of resorption after prolonged use of removable prosthesis or
tooth loss either due to trauma, periodontal disease or caries [5-9].
It is understood that after a tooth removal, the vertical bone resorption yields a 0.7 mm rate after three months [10] and
after six months, a range of 11 up to 22 per cent of loss is expected [8].
In order to have a properly functional and esthetical implant-based restoration, a minimal of 10mm bone height, a 1,8
mm of buccal plate and a 1 mm of palatal plate left after implant placement are required [11].
Whenever the bone volume precludes the implant placement due to the inadequate vertical height one should make use
of surgical vertical ridge augmentation [1,2,7,8,10-12]. Other solutions rather than the surgical ones may include short
implants, tilted implants or the use of implant based prothesis with artificial gingiva [10].
As far as the surgical procedures are concerned, the options are guided bone regeneration, osteogenesis distraction, tent
pole, inlay and only bone blocks [1,2,7,11,12].
Most of the augmentation procedures demand grafting material, which can be autogenous, alloplastic, xenogenous or
allogenous. The golden standard of these materials remain the autogenous graft because of its osteogenic, osteoinductive
and osteoconductive properties [5,7].
Regardless of the surgical technique of choice, the practitioner must pay attention to the PASS principals, namely: Primary closure, Angiogenesis, Space and Stability [1].
Vertical ridge augmentation is considered as an arduous and challenging surgical procedure [10].
The SBB technique is an augmentation procedure in which autogenous grafts are used for both vertical and horizontal
augmentations [3]. Thin bone blocks combined with particulated bone are used for reconstruction so that the regeneration time of the augmented site is enhanced due to better revascularization e regeneration capabilities of the graft [3].
Case Report
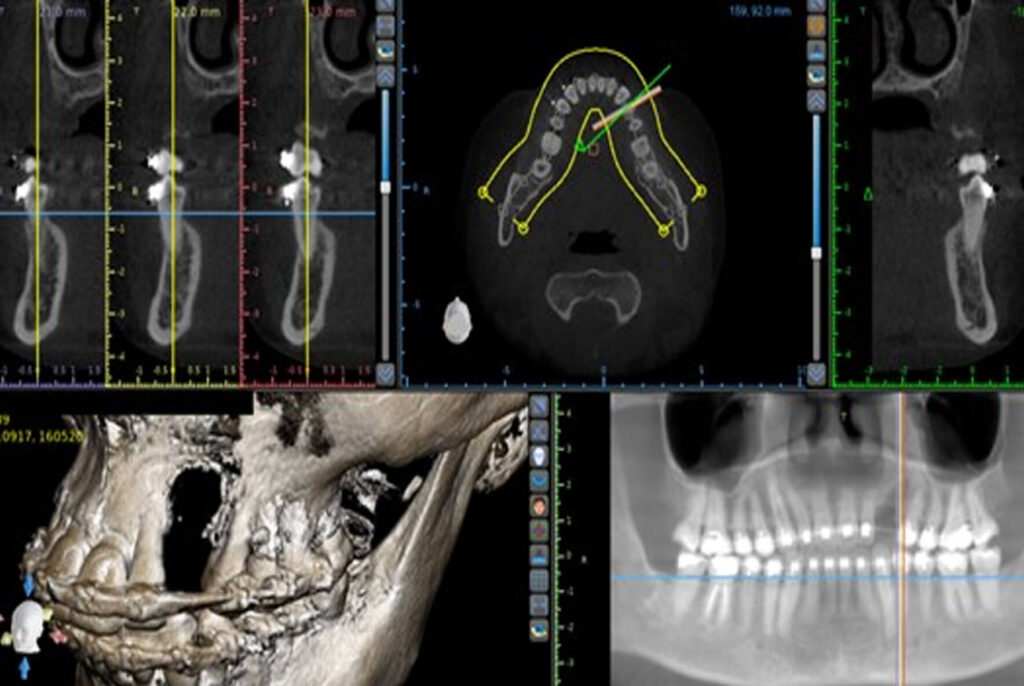
A 30-year-old female patient was referred for an implant restoration in the left upper canine area. In order to acquire a
precise assessment of the tridimensional bone volume, a Cone Beam CT scan was taken which revealed a vertical osseous deficiency (fig 1). Prior to the implant installation a surgical vertical augmentation became necessary so that the
implant could be placed in a tridimensional correct position (fig 2).
Her medical examination revealed no comorbidities or allergies. Besides, she was under orthodontical treatment to
improve her occlusion and gain a proper rehabilitation space.
The Split Bone Block technique was the surgery of choice for the vertical augmentation prior to the implant installation
and the autogenous bone was harvested from the left ramus.
The surgery was carried out under local anaesthesia with Articaine 4% and 1:100.000 epinephrine. A 0,12% Chlorexidine was prescribed preoperatively along with 1mg Amoxicillin and 8mg Dexamethasone P.O. 1 hour before surgery.
A mucoperiosteal envelope incision was executed with a number 15C scalpel from the right central incisor to the left first
premolar. After the detachment of the vestibular mucosa, the palatal mucosa was detached too (fig 3).

Figure 1 – CT scan showing vertical
deficiency.

Figure 2 – Intraoral aspect of the left
canine area.

Figure 3 – Vestibular e palatal flaps
released.
The bone graft was harvested on the left mandibular ramus (fig 4). A mucoperiosteal incision was made with a number
15C scalpel from the mandibular ramus to the mandibular vestibulum by the first molar. After the detachment of the
vestibular mucosa, the lingual mucosa also was detached.
Two vertical and one horizontal osteotomy were executed on the mandibular ramus with a 701 bur so that a bone block
could be harvested for the vertical reconstruction (fig 5). Following the graft removal with the aid of a root elevator, the
block was cut into two thin pieces with a disc and the remain bone was milled, so that it could be used as particulated
bone (figs 6 to 8).

Figure 4 – Donor site = left ramus.

Figure 5 – Osteotomies performed
before graft removal.

Figure 6 – Bone block harvested
from donor site

Figure 7 – Block cut into 2 pieces
with the aid of a disc.

Figure 8 – Bone plates cut to adapt
to the vestibular e palatal aspects of
the recipient site

Figure 9 – Bone plate adapted to
the palatal aspect of the recipient
site.
Two blocks were loosely fixed from the vestibular and palatine canine area with two 1.5 x 10mm ostheosynthesis screws
(Orth screws – Implacil de Bortoli, Sa o Paulo – Brazil) and the particulated bone was inserted into the gap among the
plates (figs 9 to 12).
Subsequently, a conjunctival pedicled graft was rotated from the ipsilateral palate in order to cover the autogenous graft
(fig 13).
The wound was closed with a 5-0 polypropylene suture, which was removed after 15 days (fig 14). The surgery healed
uneventfully (fig 15). The patient was prescribed post operatively with amoxycillin 500 mg P.O. every 8 hours for seven
days and Ibuprofen 600 mg every 6 hours for 5 days.
The grafted site was reopened, and the implant placed 4 months after the augmentation (fig 16)

Figure 10 – Palatal and vestibular
plates adapted to the recipient site.

Figure 11 – Two osteosynthesis 1,5 x
10 mm screws inserted to stabilize the
plates

Figure 12 – Particulate bone inserted
between the two plates.

Figure 13 – Pedicled conjunctival
graft rotated to cover the grafted
site

Figure 14 – Surgical site sutured
Figure 15 – Post operative CT scan.

Figure 16 – Augmented bone 4 months after the initial surgery
Discussion
Vertical Ridge augmentation inflicts a greater surgical challenge and a more unpredictable postoperative result than the
horizontal reconstructions because it requires a careful flap advancement to cover the graft and stabilize the clot [9].
Two of the most usual treatment modalities for ridge augmentation are Guided Bone Regeneration (GBR) and the use of
autogenous bone blocks or Split Bone Blocks [1,6,9,10].
Besides autogenous grafts other types of grafts may be used for ridge reconstructions, such as xenogenic, allogeneic and
alloplastic grafts, even though the autogenous ones are the main biomaterial since they are the only one to be either
osteogenic, osteoconductive and osteoinductive [5,7].
Within the scope of the GBR principles, the combination of xenogenic and autogenous graft, in a 1:1 ratio is indicated,
since while the former maintains the osseous bone structure due to its slow reabsorption properties, the latter promotes
the activity of growth factors and osteoblasts [8]. Besides, aiming to enhance and maintain the space created by the surgical vertical augmentation, a nonresorbable barrier should be utilized, such as a titanium mesh or a Titanium reinforced
high density PTFE (d-PTFE) membrane [10,12-14]. Thus, the PASS principles of Space and Stability would be respected
[10,14]. Those barriers must be submerged for bone formation from 6 to 9 months of uneventful healing period till they
can be removed, and the dental implant be inserted [6]. The main disadvantage of this surgical technique is the high incidence of membrane exposure witch probably might put at risk the final result, since it is reported the in places where the
membranes are exposed the bone gain decreased six times compared to cases of nonexposed membranes [10]. Besides
the increased risk of exposure and infection, the utilization of xenogenic graft and nonresorbable membranes make the
overall treatment costs more elevated [7].
As far as the SBB technique is concerned, it employs autogenous bone mainly harvested from intraoral sites such as
ramus and chin [7]. Thin bone blocks are combined with particulate bone chips [3]. This mixture hastens the bone formation process because of the improvement of the osteoconductive properties of the graft [3]. The autogenous graft is
considered the gold standard graft for vertical reconstructions, with high success rates [3,11]. This kind of graft contains
living cells such as osteocytes and osteoblasts, along with bone morphogenetic proteins that will trigger mesenchymal
cells to turn into osteoblasts [7]. The thin bone blocks create a stable box that will be filled with particulate bone chips
and will satisfy the PASS Space and Stability requirement [3.] The dental implants can be installed after a 3-month preoperative time [3,15].
Another advantage of the SBB is the fact that there is no need to use any membrane or grafts other than the autografts.
Hence, the possibility of transmission of diseases and the appearance of allergies is abolished [7].
The thin split bone blocks increase the graft surface and volume so that there is no need to harvest grafts in extraoral
sites even in cases of extensive vertical augmentations [3].
Conclusion
The Split bone block technique is an advantageous technique in cases of vertical augmentations regardless of the volume
of reconstruction required because of the nature of the autogenous graft and the architecture of the graft that mixes thin
bone blocks and particulate bone. In addition to that, this technique is cost effective and with no risks of allergies or viral
diseases transmission since there is no need to use barriers or any kind of grafts but the autografts.
The autogenous grafts provide a more predictable result for vertical augmentations and the SBB allows implants placements
3 months after the reconstructive surgery.
Conflict of Interest
The authors declare no conflict of interest.
References
1. Sa nchez-Sa nchez, J.; Pickert, F.N.; Sa nchez-Labrador, L.; GF Tresguerres, F.; Martí nez-Gonza lez, J.M.; Meniz-Garcí a, C. Horizontal Ridge Augmentation: A Comparison between Khoury and Urban Technique. Biology. 2021; 10: 749.
2. F. Briguglio, D. Falcomata , S. Marconcini, L. Fiorillo, R. Briguglio, D. Farronato, “The Use of Titanium Mesh in Guided
Bone Regeneration: A Systematic Review”, International Journal of Dentistry. 2019; Article ID 9065423, 8 pages.
3. Khoury F, Hanser T. Three-Dimensional vertical alveolar ridge augmentation in the posterior maxilla: a 10-year clinical study. Int J Oral Maxillofac Implants 2019;34:471–480.
4. Rakhmatia YD, Ayukawa Y, Furuhashi A, Koyano K.Current barrier membranes: Titanium mesh and other membranes
for guided bone regeneration in dental applications. J Prost Res. 2013; 57(1): 3-14.
5. Soldatos N.K, Stylianou P, Koidou VP, Angelov N, Yukna R, Romanos GE. Limitations and options using resorbable
versus nonresorbable membranes for successful guided bone regeneration. Quintessence Int. 2017;48: 131-147.
6. Cucchi A, Vignudelli E, Napolitano A, Marchetti C, Corinaldesi G. Evaluation of complication rates and vertical bone
gain after guided bone regeneration with non-resorbable membranes versus titanium meshes and resorbable membranes. A randomized clinical trial Clin Implant Dent Relat Res. 2017; 19:821–832.
7. Khoury F, Doliveux R. The bone core technique for the augmentation of limited bone defects: Five-year prospective
study with a new minimally invasive technique. Int. J. Periodontics Restor. Dent. 2018; 38 (2): 199-207.
8. Vallada o Jr CA, Monteiro MF, Joly JC. Guided bone regeneration in staged vertical and horizontal bone augmentation
using platelet-rich fibrin associated with bone grafts: a retrospective clinical study. International Journal of Implant Dentistry. 2020; 6:72.
9. Windisch P, Orban K, Salvi GE, Sculean A, Molnar B. Vertical-guided bone regeneration with a titanium-reinforced dPTFE membrane utilizing a novel split-thickness flap design: a prospective case series. Clinical Oral Investigations 2021;
25:2969–2980.
10- Urban I, Monje A, Lozada J, Wang HL.Vertical ridge augmentation and soft tissue reconstruction of the anterior
atrophic maxillae: a case series. Int J Periodontics Restorative Dent. 2015;35: 613-623.
11. El Zahwy M, Taha Said Abdallah K., Mounir R, Mounir M. Assessment of vertical ridge augmentation and marginal
bone loss using autogenous onlay vs inlay grafting techniques with simultaneous implant placement in the anterior maxillary esthetic zone: A randomized clinical trial. Clin Implant Dent Relat Res. 2019;1–8.
12. Mounir M, Mounir S, Elfetouh A, Shaker M. Assessment of vertical ridge augmentation in anterior aesthetic zone using onlay xenografts with titanium mesh versus the inlay bone grafting technique: A randomized clinical trial. Int. J. Oral
Maxillofac. Surg. 2017; 46 (11): 1458-1465.
13. Rakhmatia YD, Ayukawa Y, Furuhashi A, Koyano K. Current barrier membranes: Titanium mesh and other membranes for guided bone regeneration in dental applications. Journal of Prosthodontic Research. 2013;57: 3–14.
14. Naung NY, Shehata E, Van Sickels JE, Resorbable Versus Nonresorbable Membranes When and Why. Dent Clin N Am
63. 2019; 419–431.
15. Khoury F, Hidajat H. Extensive autogenous bone augmentation and implantation in patients under Bisphosphonate
treatment: A 15-case series. Int J Periodontics Dent 2016; 36: 9-18.