João C. Vicente de Barros Jr. , Fabrício L. Gebrin , Jamil A. Shibli , Márcio de Carvalho Formiga ,
Tárcio H. Ishimine Skiba
1. Department of Implantology and Oral Rehabilitation, SOEP, Porto Velho, BRA 2. Department of Periodontology, UnG, Guarulhos, BRA 3. Albert Einstein Israelite Faculty of Health Sciences, Albert Einstein Israelite Hospital, São Paulo, BRA 4. Oral Implantology, Univali São José, Florianopolis, BRA 5. Department of Pharmaceutics,, Univali, Itajaí, BRA
Corresponding author: Márcio de Carvalho Formiga, marciocformiga@gmail.com
Abstract
Abstract
Implant-supported fixed rehabilitations are a reliable solution to restore aesthetics and function to
edentulous patients. Currently, practitioners can use digital flow with CAD/CAM technology to enhance
their productivity by reducing working time and providing more comfort to patients. This study aims to
report a clinical case in which the digital flow was used to restore the inferior edentulous arch in a 55-yearold female patient with an implant-based Misch´s FP3 denture. Digital technology provides tridimensional
planning, surgical computed guides, and printed temporary rehabilitation. This case report portrays the
feasibility and ease that the digital flow provides for both surgeon and patient.
Categories: Dentistry
Keywords: implant osseointegration, 3d printing, digital workflow, virtual planning, guided implant surgery
Introduction
Prosthetic rehabilitation of patients with total edentulism remains one of the main challenges in dentistry.
The practitioner ought to restore function and esthetics most predictably while employing the shortest and most comfortable working time, sometimes without important clinical parameters to aid rehabilitation [1,2]. The implant-supported full arch fixed rehabilitation has become an accepted treatment option for such cases, more specifically in immediate loading cases, thanks to the evolving technology in all the fields of digital dentistry, assuring more predictability and precision in oral rehabilitation [3]. Regarding evolving technology, digital workflow may provide a virtual tridimensional preoperative planning, where we can visualize the final restoration before it starts, in addition to a 3D printing surgical guide and the possibility of printing a temporary prosthesis before the surgical phase [4,5]. The use of this technology may decrease the need for many appointments and, at the same time, ensure more accuracy in the final result.
The main advantage of digital planning and the utilization of a surgical guide is the possibility of placing the dental implants in an optimal tridimensional position, which is a key point to a long-term successful case.
Computer-guided, flapless implant surgery offers the advantages of high-precision implant placement,
shorter surgical time, less trauma and bleeding, and fewer postoperative complications. It is, however, a
highly technique-sensitive procedure at all stages that begins with the virtual planning and finishes with the surgical procedure, all of which need to be accurately performed [6].
Therefore, this study reported a clinical case of a full-arch rehabilitation, screw-retained on five 3D-printed implants, placed by computer-guided surgery, and submitted to an immediate loading protocol, and the 24- month follow-up.
Case Presentation
A patient, 55-year-old, female, was referred to the clinic of the Department of Implantology and Oral
Rehabilitation at Study, Research and Dental Service (SOEP), to treat her lower jaw with a screw retained full arch rehabilitation over implants. In the intra-oral examination, we could observe that she presented only the right first and second premolars (Figure 1). The choice of full-arch rehabilitation with the flapless
placement of five 3D-printed implants, followed by immediate loading, was proposed and accepted by the patient, who used to have a removable partial denture, and wanted a fixed alternative for her rehabilitation, with minimal surgeries possible.
The full digital workflow was utilized in this case to improve predictability and long-term stability and
decrease the clinical steps to rehabilitation completion.
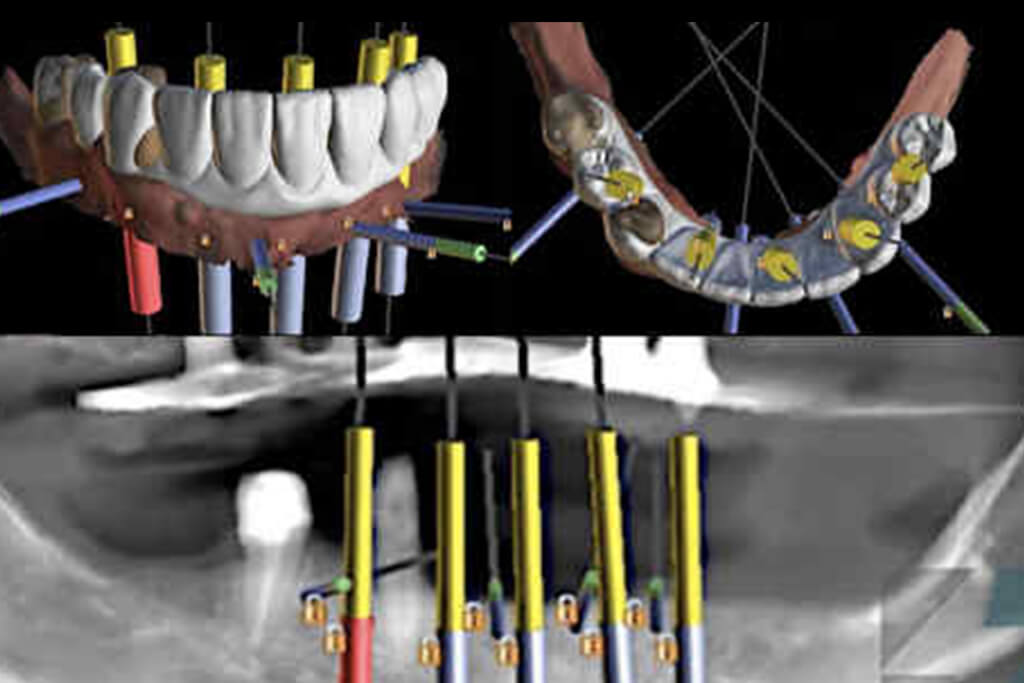
After intraoral scanning, the case was digitally planned using CT scan and computer software that granted a tridimensional view of the arches and consequent assessment of the ideal tridimensional position of five dental implants placed at the inter-foraminal region (Figure 2). A set of surgical stackable guides was printed to be used intraoperatively, aimed to guide the optimal tridimensional flapless implant placement with immediate loading (Figure 3). Four 3.5 x 11.5 mm implants and one 4 x 10 mm (Plenum Bioengenharia- SP, Brazil), commercially produced by additive manufacturing, using titanium powder grade 23, were planned. The patient approved the treatment plan and provided a written term of free and informed consent to
publish this report.
The surgery was performed under local anesthesia, with 2% Articaine and 1:100.000 epinephrine. The
patient was prescribed with 0.12% Chlorexidine rinse right before surgical draping. One hour prior to the
procedure, 8 mg dexamethasone and 1 gm of Amoxicillin were prescribed. Moreover, 500 mg of Amoxicillin every 8 hours for 7 days and Ibuprofen 600 mg every 6 hours for 3 days postoperatively for pain control were prescribed.
After anesthesia, two stackable guides were installed in the lower jaw. The first one with 3 pin and the
second through magnets on the top of the other, so that three 3.5 x 11.5 mm implants could be placed on a flapless approach (Figures 4 – 6). Subsequently, the magnet-inserted implant guide was removed, and the teeth that aided in the stabilization of the first guide were extracted with minimal trauma, along with the performance of a small osteoplasty in the first premolar alveolus employing a hand-piece spherical bur (Figures 7 and 8).
A second guide was placed by means of magnets so as to guide the placement of a 4 x 10 mm implant in the first right premolar area, whereas a 3,5 x 11,5 mm implant could also be placed in the second right premolar alveolus (Figures 9 – 11).
The 3D digital planning also allowed the crafting of a resin (Makertech) printed temporary fixed prosthesis
(Figure 12), which was installed intraoperatively after the abutment installation in all implants and the use
of flowable resin to fill the gaps between the provisional prosthesis and the titanium provisional cylinders
(figure 13), before the removal of the surgical guide (Figure 14). After the proper resin polishing and
adjustments (Figure 15), the fixed screw retained temporary prosthesis was installed over the abutments
(Figure 16 and 17) and the patient had aesthetics and function restored immediately after surgery (figure
18).
The patient was instructed to apply ice bags to the surgical area for 48 hours, for approximately 15 minutes every hour, and to eat only soft foods. On the day after surgery, the patient suspended the medication because she had no pain.
After 4 months the patient returned and the temporary prosthesis was replaced for a final full arch screw
retained zirconia rehabilitation (Figure 19-21).
After 24 months, a Cone Beam Computed Tomography was requested for the patient for radiographic control of the implants and the surrounding bone (Figure 22), showing great stability of the peri-implant hard tissue. The peri-implant mucosa was noted to be healthy, without bleeding on probing. Peri-implant sulcus depth was lower than 3 mm, even around the left distal implant, that don’t have a satisfactory keratinized tissue band, showing that the patient was able to maintain proper hygiene under the prosthesis.
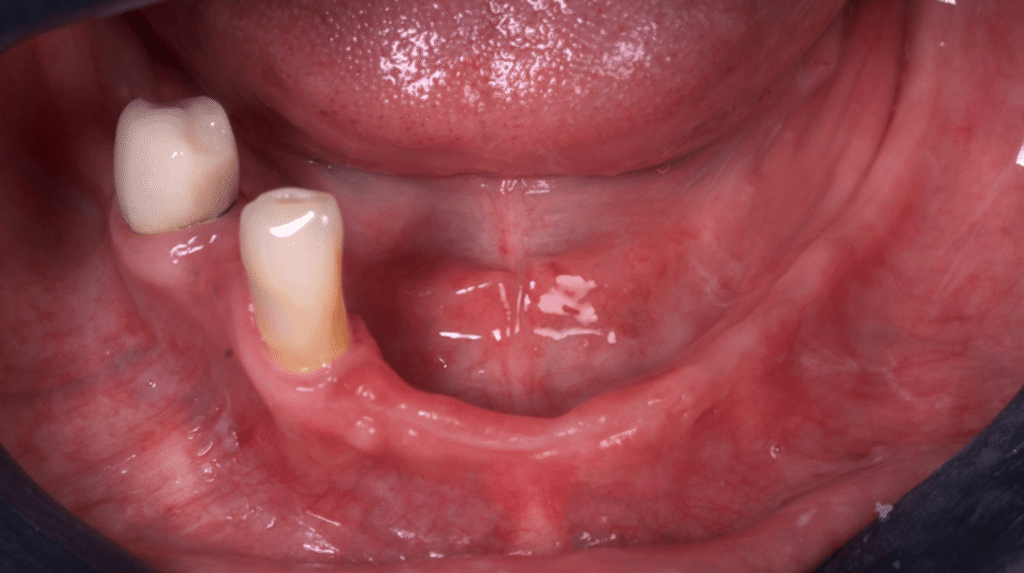
FIGURE 1: Intra oral view of the mandible
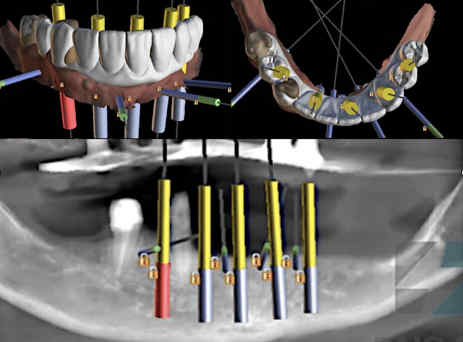
FIGURE 2: 3D digital planning of the implants (Raio 3D- Porto Velho,
Brazil)
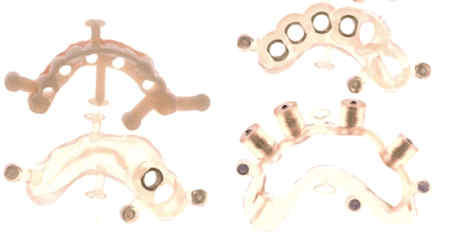
FIGURE 3: Set of stackable guides utilized for this clinical case
(Makertech Maquira. São Paulo, Brazil)
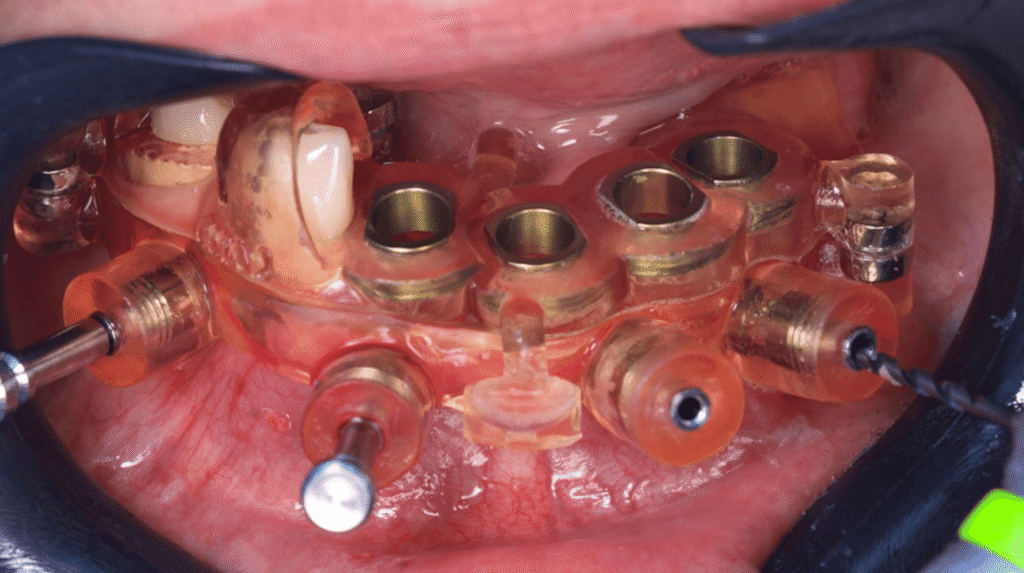
FIGURE 4: Buccal view of the two stackable guides installed and
stabilized with 3 pins

FIGURE 5: Implant placement through the printed surgical guide
(Plenum. Jundiaí, Brazil)

FIGURE 6: Flapless placement of the second implant
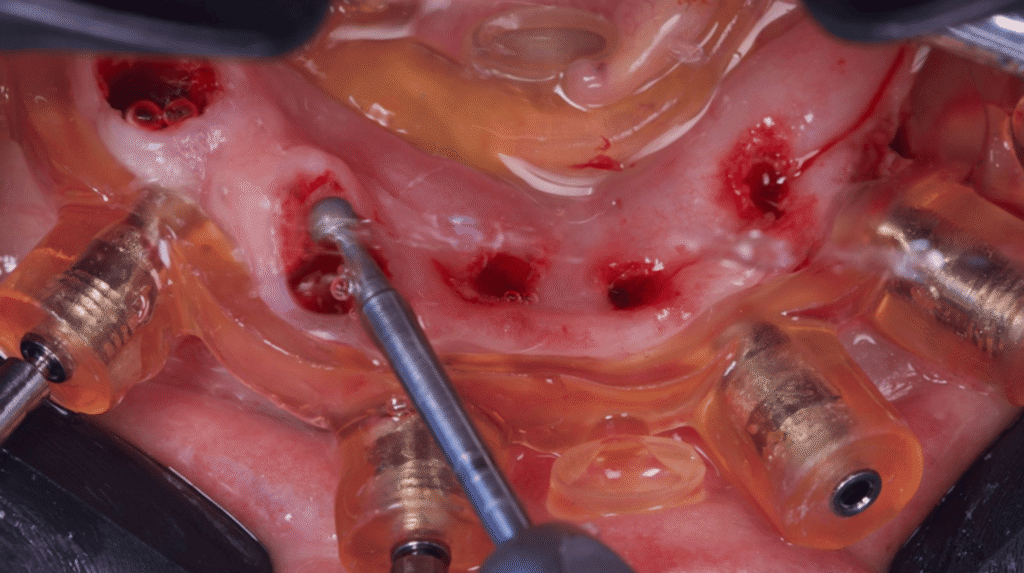
FIGURE 7: Osteotomy of the alveolus after teeth extraction (SupremoSão Paulo, Brazil)
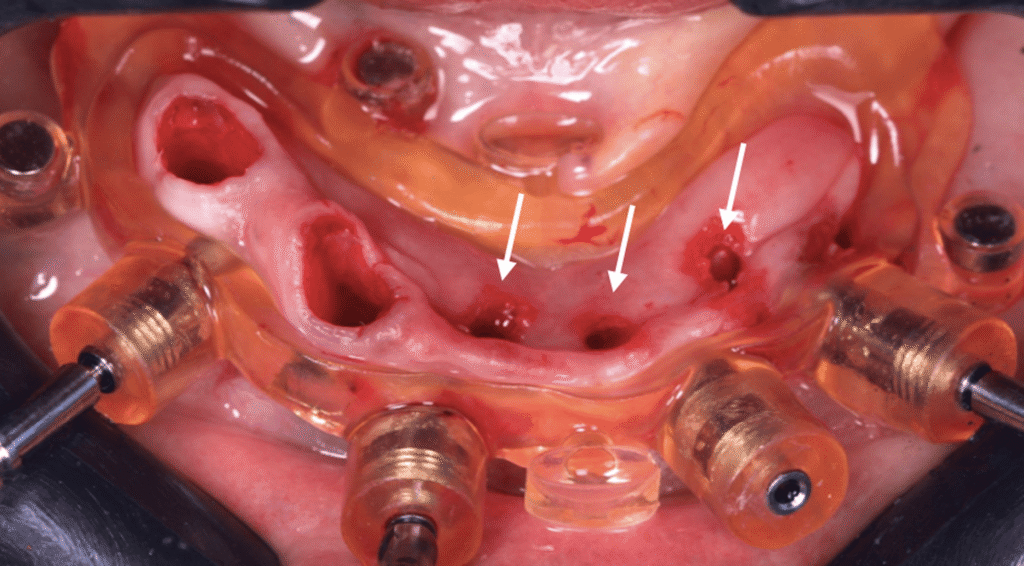
FIGURE 8: View of the lower jaw mucosa after osteoplasty and 3
implants placed (white arrows)
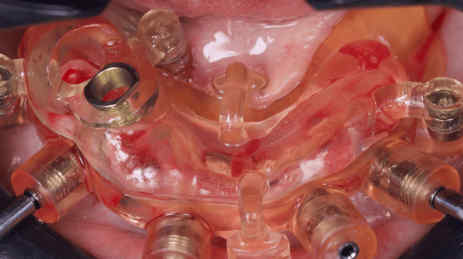
FIGURE 9: Second guide placed in position by magnets

FIGURE 10: Placement of an 3D implant in the first right premolar
alveolus
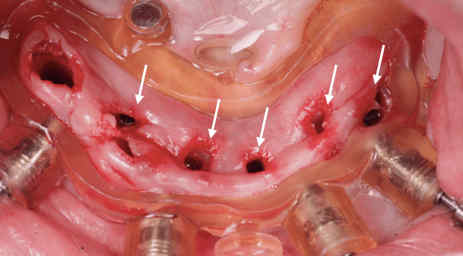
FIGURE 11: View of the lower jaw mucosa after all implants have been
placed (white arrows)
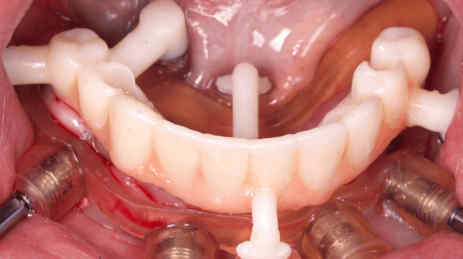
FIGURE 12: View of the resin printed temporary prosthesis installed
over the surgical guide still in position (Raio 3D- Porto Velho, Brazil)

FIGURE 13: Capture of titanium cylinders to the temporary prosthesis
with flow-resin

FIGURE 14: Oclusal view of the mucosa with the mini-abutments
installed in the implants after removal of the surgical guides and
temporary prosthesis

FIGURE 15: Filling of the gaps between the titanium cylinders and the
temporary prosthesis with flowable resin (left) and stackable pins
removal (right) (EFF- São Paulo, Brazil)

FIGURE 16: Oclusal view of the temporary fixed screw retained
prosthesis installed

FIGURE 17: Buccal view of the temporary fixed screw retained
prosthesis installed

FIGURE 18: Extra oral view of the esthetics restored immediately after
surgery

FIGURE 19: Buccal view of the mucosa and abutments after removal of
the temporary prosthesis

FIGURE 20: View of the zirconia rehabilitation before installation

FIGURE 21: Buccal view of the zirconia fixed rehabilitation installed
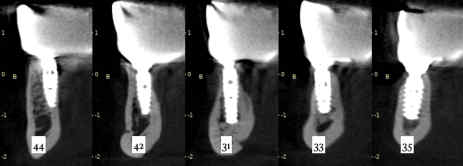
FIGURE 22: 24 months cone beam computed tomography follow-up of
the implants (Raio 3D- Porto Velho, Brazil)
Discussion
Advances in 3D digital planning in implantology are not limited to planning implant positions, producing
computed surgical guides, or preparing prosthetic rehabilitation even before surgery, with reliable accuracy, as we presented in this case. Digital workflow has become in the 21st century a part of the dental offices and laboratories’ daily routine, such as intraoral digital scanning, virtual planning, guided surgery, and 3D printing [2,3,7,8]. Also, intraoral scanning has a vast advantage over conventional impression, considering that it is more comfortable for the patients, saves time and costs, besides avoiding mishaps like gypsum model fracture or loss [2,3,9,10]. In this case report, we could use most of the advantages of the latest digital workflow to deliver the fixed rehabilitation over implants more predictably, faster, and with more comfort to the patient.
The surgical stackable guides warrant a faster and more precise surgical procedure, decreasing the transoperative and post-operative morbidity since the surgeon can perform a flapless implant placement with a safer predictability of the distance between the implant and important anatomical structures such as the maxillary sinus and inferior alveolar nerve [10]. A flapless computed-guided surgery promotes greater comfort during and after the procedure. With such predictability, we could perform an immediate loading procedure with the installation of the temporary prosthesis intra-operatively, immediately after placement of the implants and abutments [6,8]. As a consequence, the patient finishes the surgery with function and aesthetics restored [10].
Computer-guided, flapless implant surgery offers the advantages of high-precision implant placement,
shorter surgical time, less trauma and bleeding, and less postoperative inflammation, edema, and
hematoma. Among the disadvantages of flapless surgery, we can cite that it does not consider the soft tissue quality, and in certain situations, some of the implants may be placed in areas with little or no keratinized tissue [4,6,10]. In this case report, only one of the implants was placed in a region with minimum keratinized tissue, and needs more attention on the peri-implant health maintenance.
This case report described the placement of commercially available titanium dental implants produced by
additive manufacturing (direct metal laser sintering). The layer-by-layer build-up of 3D printed implants
offers versatility, accuracy, better mechanical properties, and enables better control of the implant micro
and nano-geometry [11]. A recent study [12] showed a similar case report with a 24-month follow-up that
used the same implant manufacturer, with soft and hard peri-implant tissue stability along this period. The
same results were shown in our case report, with a different approach to the material in the prosthetic
phases, both temporary and zirconia rehabilitation.
The combination of digital planning with the development of new technologies, such as dental implants
produced by additive manufacturing, improved the bone response, facilitating wound healing in the early
stages of osseointegration [13,14]. Previous studies in humans [13,14] and animals [15] showed that titanium implant surface topography produced by the 3D printed technology provided an increased bone volume and higher rates of bone-to-implant contact, resulting in a stable bone anchorage.
Conclusions
The digital flow in implantology provided a better quality in this presented rehabilitation, since it improved
the predictability and long-term stability of the implant-based rehabilitation. Furthermore, the patient was
treated more rapidly and with less morbidity due to the possibility of a flapless implant placement procedure along with a shorter overall treatment time.
Additional Information
Disclosures
Human subjects: Consent for treatment and open access publication was obtained or waived by all
participants in this study. Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all
authors declare the following: Payment/services info: All authors have declared that no financial support
was received from any organization for the submitted work. Financial relationships: All authors have
declared that they have no financial relationships at present or within the previous three years with any
organizations that might have an interest in the submitted work. Other relationships: All authors have
declared that there are no other relationships or activities that could appear to have influenced the
submitted work.
References
- Jafarpour D, El-Amier N, Feine J, et.al : 3D printing vs traditional workflow for the fabrication of
mandibular implant overdentures: study protocol for a mixed-methods cross-over RCT. Trials. 2024, 16:267. 10.1186/s13063-024-08097-7 - Seth C, Bawa A, Gotfredsen K: Digital versus conventional prosthetic workflow for dental students
providing implant-supported single crowns: A randomized crossover study. J Prosthet Dent. 2024, 131:450- 10.1016/j.prosdent.2023.03.031 - Rotaru, C.; Bica, E.A.; Butnarasu, C.; Sandulescu, M: Three-Dimensional Scanning Accuracy of Intraoral Scanners for Dental Implant Scan Bodies—An Original Study. Medicina. 2023, 59:2037.
10.3390/medicina59112037 - Canullo L, Pesce P, Caponio VCA, et. al : Effect of auxiliary geometric devices on the accuracy of intraoral scans in full-arch implant-supported rehabilitations: An in vitro study. . J Dent. . 2024, Jun:104979.10.1016/j.jdent.2024.104979
- Tahayeri A, Morgan M, Fugolin AP, et.al : 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent Mater. 2018, 34:192-200. 10.1016/j.dental.2017.10.003
- Manfredini M, Poli PP, Maiorana C, Salina FE, Tandurella M, Beretta M: Computer Aided Full Arch
Restoration by Means of One-Piece Implants and Stackable Guide: A Technical Note. Dent J (Basel. 2023, 1:256. 10.3390/dj11110256 - Altarazi A, Haider J, Alhotan A, Silikas N, Devlin H: Assessing the physical and mechanical properties of 3D printed acrylic material for denture base application. Dent Mater. 2022, 38:1841-1854.10.1016/j.dental.2022.09.006
- Martins J, Rangel J, de Araújo Nobre M, Ferro A, Nunes M, Almeida R, Moura Guedes C: A New Full Digital Workflow for Fixed Prosthetic Rehabilitation of Full-Arch Edentulism Using the All-on-4 Concept. Medicina (Kaunas). 2024 Apr. 26:720. 10.3390/medicina60050720
- Minervini G, Franco R, Crimi S, et. al: Assessment of fully digitalized workflow for implant-prosthetic
rehabilitation in temporomandibular disorders patients: A clinical study. Saudi Dent J. 2023, 35:684-691.10.1016/j.sdentj.2023.05.024 - Todaro C, Cerri M, Rodriguez Y Baena R, Lupi SM: Full-Arch Guided Restoration and Bone Regeneration: A Complete Digital Workflow Case Report. Healthcare (Basel. 2023, 2:1301. 10.3390/healthcare11091301
- Goguta L, Lungeanu D, Negru R, et. al: Selective laser sintering versus Selective laser melting and Computer aided design – Computer aided manufacturing in double crowns retention. J Prosthodont Res. 2021, 65:371-10.2186/jpr.JPOR_2019_556
- de Carvalho Formiga M, Fuller R, Ardelean LC, Shibli JA: Immediate Loading Full-Arch 3D-Printed ImplantSupported Fixed Rehabilitation: A Case Report with 24-Month Follow-Up. Medicina (Kaunas. 20242,60:1614. 10.3390/medicina60101614
- Shibli JA, Mangano C, Mangano F, et. al: Bone-to-implant contact around immediately loaded direct laser metal-forming transitional implants in human posterior maxilla. J Periodontol. 2013, 84:732-7.
10.1902/jop.2012.120126 - Lang NP, Imber JC, Lang KN, Schmid B, Muñoz F, Bosshardt DD, Saulacic N: Sequential osseointegration of a novel implant system based on 3D printing in comparison with conventional titanium implants. Clin Oral Implants Res. 2023, 34:627-638. 10.1111/clr.14072
- Shibli JA, Formiga MC, Elias GA, et. al: Impact of Implant Surface and Smoking on Peri-Implant Human Bone: What we Learned from The Last 20 Years?. Braz Dent J. 2024 Oct. 25:246115. 10.1590/0103-6440202406115